Diaphyseal Humerus Fracture with Intramedullary Nail
This article accompanies the video of the surgery narrated by Dr. Sávio Chami and describes in detail the surgical technique for the treatment of diaphyseal humeral fractures using an intramedullary rod. We will cover everything from the initial planning and patient positioning to the stages of reduction, instrumentation, and closure. The aim is to provide a technical and educational guide to optimize the understanding of the procedure.
Technique Priorities
The technique prioritizes:
- Appropriate reduction of fragments
- Preservation of soft tissues
- Precision in the creation of the entry portal
Indication and Objectives
The intramedullary rod may be indicated for diaphyseal fractures of the humerus, and the demonstrated method was planned to:
- Achieve precision in the creation of the entry portal
- Reduce surgical trauma
- Facilitate the performance of the procedure
Surgical Technique
1.Intraoperative Positioning and Planning
With the patient positioned in the supine position and the head elevated to approximately 40 degrees, the procedure begins with marking the long axis of the humerus (medullary canal), identifying the deformity and the exact location of the fracture with a dermographic pen.
2. Reduction and Placement of the Guide Wire (Joystick)
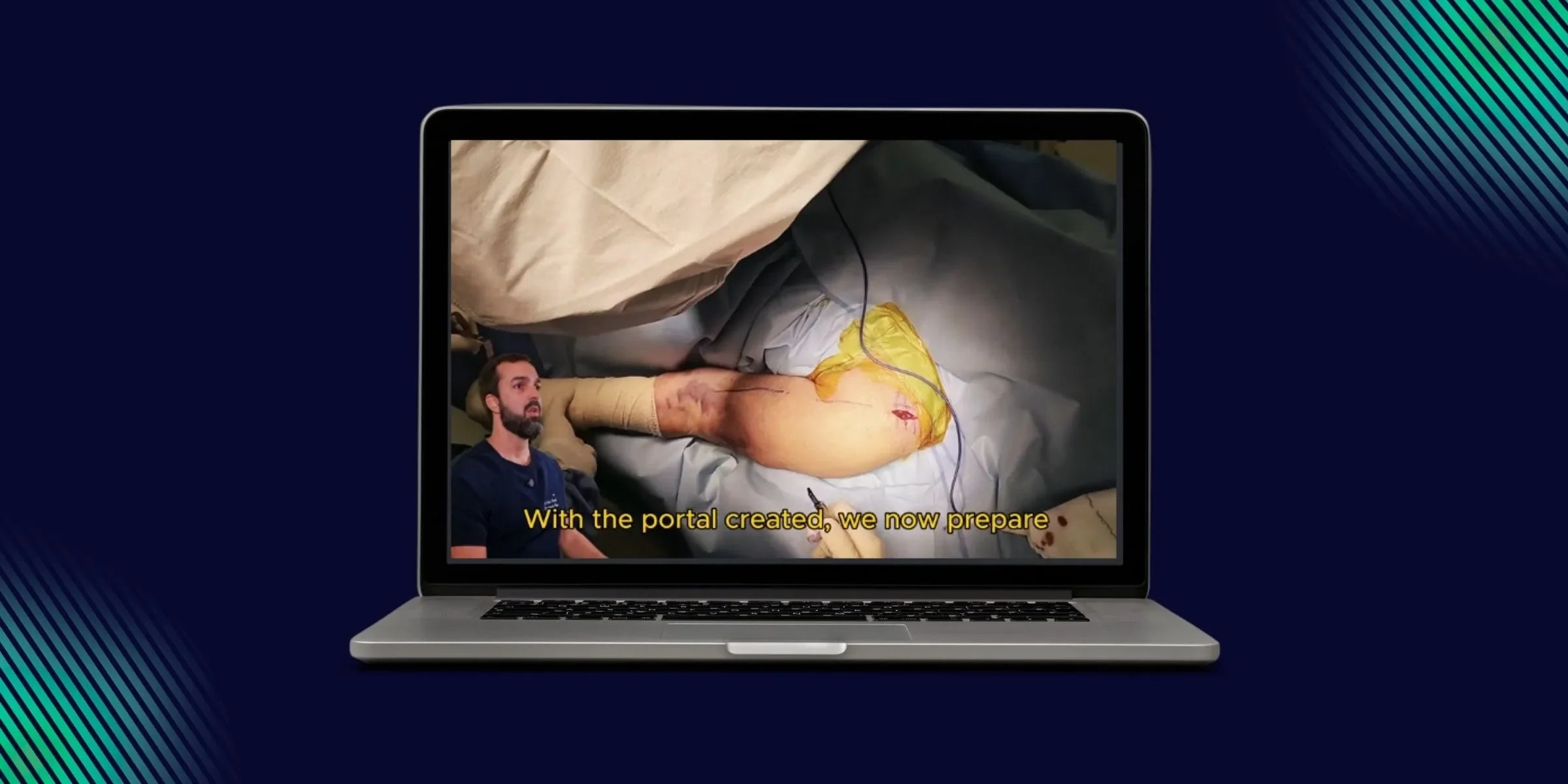
A portal of access is created aligned with the diaphysis, with special attention to the rotator cuff. The entry should be made in the direction of the fibers of the rotator cuff, never transversely, to avoid residual pain post-procedure due to compromise of the rotator cuff. After the portal is created, preparations are made to achieve an ideal angle of attack for the entry of the guide wire.
Joystick Technique
A hole is made in the posterolateral region of the shoulder for the insertion of a Kirschner wire of 3.0mm or 2.0mm.This wire will serve as a "joystick" to:
- Assist in the adduction of the upper fragment
- Expose the entry point
- Correct the rotation
The maneuver with the joystick allows for complete mobilization of the proximal fragment pulled by the deltoid, correcting the abduction and facilitating a precise entry angle at the top of the humeral head, at the transition between the greater tuberosity and the humeral head (predominantly at the head of the humerus)
Ideal Entry Point
The introduction of the guide wire should be directed predominantly at the humeral head, avoiding the tubercle-head transition to prevent a possible fracture of the greater tuberosity during the widening of the entry point.
The radiographic evaluation of the entry point is performed with the joystick itself, in anteroposterior and lateral incidences, as the proximal fragment is free, allowing for direct and accurate visualization of the entry. This approach is more effective than elbow rotation for obtaining the lateral incidence, which can produce inaccurate images.
3. Creation of Entry for the Medullary Canal and Insertion of the Rod
The joystick is removed to proceed with the drilling and introduction of the intramedullary rod. After the guide wire is passed, the rod is measured.
⚠️ Important Attention: The medullary canal at the end is triangular, making measurement with the wire less accurate. It is recommended to apply a discount to compensate for the tapering of the medullary canal, preventing the rod from being prominent.
4.Blocking and Finalization
Proximal Blocking
After the introduction of the intramedullary rod, the proximal blocks are created using oblique screws directed to the humeral calcar.
Distal Blocking
The distal block is performed freehand, being a highly difficult procedure due to the anatomical characteristics of the distal humerus, which has a triangular anterior face.
Important Technical Tips:
- Use a drill with a sharp tip to prevent slipping on the triangular apex of the anterior cortex of the humerus
- Notify the supplying company to bring a new drill with a sharp tip
- The incision for the distal block is approximately one centimeter
Finalization
After placing the distal block and removing the introducer and guide, the diaphyseal fracture with a spiral line is observed to be satisfactorily reduced, with the implant not prominent. The rotator cuff is sutured (the incision was made along the fibers), which prevents issues with shoulder function. Proceed with subcutaneous and skin closure.
Post-operative: Results and Considerations
In the post-operative phase, the procedure allows for some mobility, providing:
- Stable reduction
- Preservation of soft tissues
- Faster functional recovery
Practical Summary of the Procedure
Surgical Checklist
- Marking: Delimit the long axis of the humerus with a dermographic pen (guide for the introduction of the guide wire in the antero-posterior view)
- Access: Create a portal aligned with the diaphysis, in the direction of the fibers of the rotator cuff
- Joystick (Kirschner Wire): Used to promote adduction, correct the rotation of the proximal fragment, and assist in checking the entry portal in the lateral radiographic view, allowing for the establishment of an appropriate entry point for the introduction of the rod
- Entry Point: Insert further towards the humeral head, avoiding the head-tuberosity transition.
- Measurement of the Rod: Account for the tapering of the medullary canal to avoid prominence of the implant.
- Blockages: Perform proximal blockages (screws oblique to the calcaneus) and distal (pay attention to the sharp drill due to the triangular anatomy)
- Closure: Suture of the cuff and skin closure
Conclusion
The intramedullary rod technique for diaphyseal humeral fractures, as demonstrated, offers a safe and precise approach. Care in the creation of the entry portal, respect for soft tissues, and attention to technical details contribute to the execution of a safe and precise procedure.
To continue staying updated with practical content directed towards surgical routines, access the Bone Reconstruction platform and explore a variety of training focused on orthopedic trauma surgeries, developed for professionals working in reconstruction and care of the musculoskeletal system.